Medicaid Managed Care
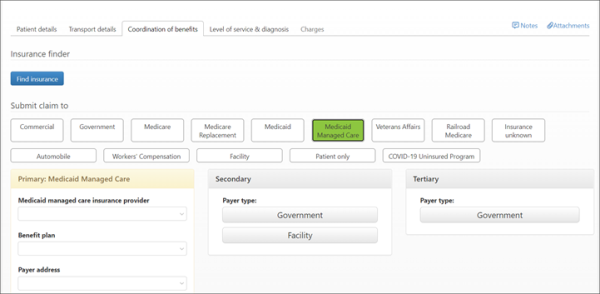
When the "Medicaid Managed Care" policy type is configured for a payer, a tile on the COB will display right after the Medicaid tile. You cannot add a Medicaid and Medicaid Managed Care plan in the COB at the same time. Medicaid Managed Care can be posted as primary, secondary, and/or tertiary.
How to administer Medicaid Managed Care
Payers will not automatically show up as Medicaid Managed Care, you will need to add this type to the payers/benefit plan before this will happen. In addition, benefit plans cannot be changed to Medicaid Managed Care, instead you must disable the existing plan and add a new one.
To administer this new policy type:
-
Click Payers on the navigation bar.
-
Find the Medicaid payer on the list and then click the payer name.
-
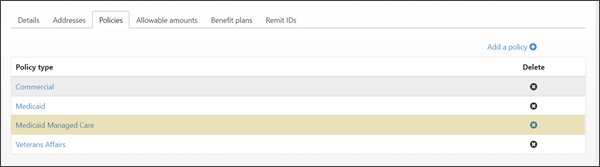
Click the Policies tab and then click Add a policy.
-
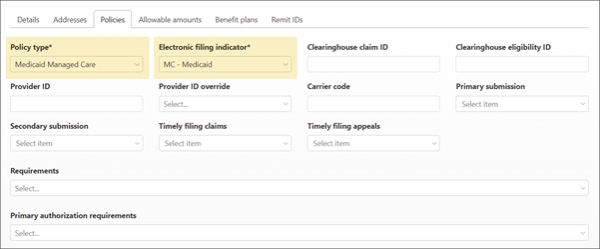
Click on the Policy typefield and select Medicaid Managed Care.
-
Click the Electronic filing indicator field and select the appropriate indicator. In most cases the indicator will be "MC-Medicaid."
-
After completing the rest of the necessary fields, click Save & close. The new policy will display in the list under the Policies heading.